Abstract
Purpose: 10-15% of adolescent and young adults (AYA) with high-risk pre-B acute lymphoblastic leukemia (ALL) may need treatment for relapsed/refractory leukemia, leading to impaired fertility. While hospitalized, sperm banking may be difficult for a newly-diagnosed AYA with ALL. This study examined practices and specific barriers to offering sperm banking at initial ALL diagnosis prior to starting chemotherapy.
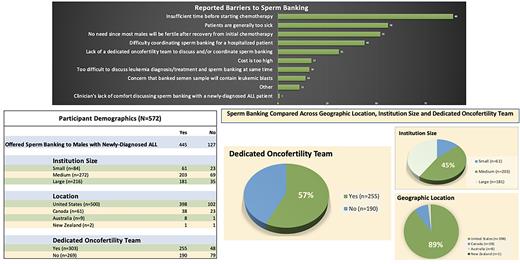
Methods: This cross-sectional survey study was distributed by email to all Children's Oncology Group (COG) oncologists (n=2345) in the United States, Canada, Australia and New Zealand from January-April 2022. Data were collected regarding size of program and institutional practices for sperm banking. Program size was defined by the total numbers of new ALL diagnoses per year: small (<10 per year), medium (10-30) or large (>30 per year). Data were summarized with counts and percentages and compared between groups using chi-square tests or Fisher's exact tests.
Results: 572 surveys were completed, representing a 25% participation rate. 78% of responders offer sperm banking to physically able males with newly-diagnosed ALL prior to starting chemotherapy. Commonly reported barriers were: insufficient time before chemotherapy (70%), patients being too sick (44%), and lack of perceived need since most will be fertile after initial treatment (41%). 57% of the total responders work at an institution with a dedicated oncofertility team. Of the 445 responders who offer sperm banking, 190 (43%) work at programs without a dedicated oncofertility team. Most (86%) responders who offer sperm banking work at medium/large-sized institutions.
Conclusion: A majority of COG oncologists who responded to our survey offer sperm banking prior to starting chemotherapy. The most frequently-cited barriers included insufficient time before treatment and patients being too sick. It is encouraging that 43% of individuals who offer sperm banking work at institutions without a dedicated oncofertility team. Medium/large institutions may have more resources to facilitate sperm banking in this setting. A possible study limitation may be respondent-bias towards individuals passionate about fertility preservation who have already adopted the practice of sperm banking at diagnosis and are not representative of all pediatric oncologists. Future directions include obtaining additional insight into COG oncologists who did not respond in order to improve education and best practices around offering sperm banking to AYA with newly-diagnosed high-risk ALL regardless of institution size or dedicated fertility preservation team.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal